View our collection of informercials below to learn more about CoCM and how it’s being implemented in practices statewide! Click on each image to be redirected to the video site. 



 .
. 
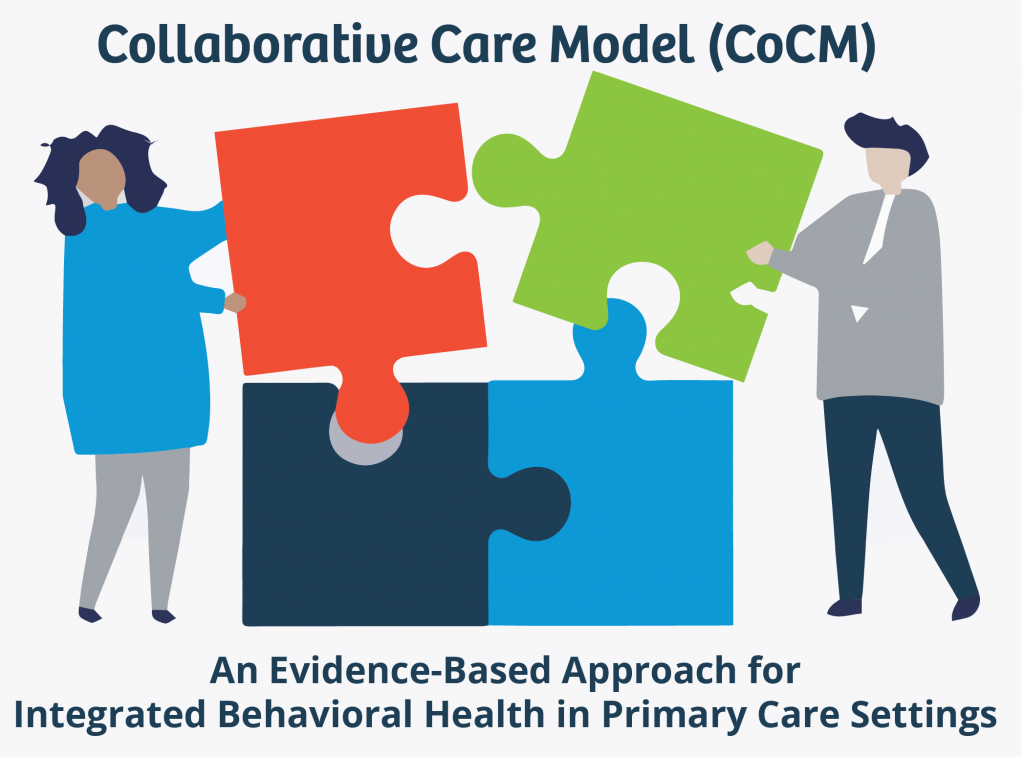
What is the Collaborative Care Model (CoCM)?
Collaborative Care Model (CoCM) is an integrated modality that provides patients with medical and behavioral health care in a primary care setting. An increasing number of primary care settings are incorporating behavioral health services. Benefits of CoCM include better patient outcomes, improved patient and provider satisfaction, and reduction in health care costs. In addition, using CoCM may reduce health disparities in access to behavioral health. Most payors in North Carolina already cover the CoCM billing codes.
The Collaborative Care Model leverages a team-based, interdisciplinary and systematic approach to screen, diagnose, treat, and provide follow-up care. The CoCM includes:
• A team made up of a Primary Care Provider (PCP) who leads the team, a Behavioral Health Care Manager (BHCM), and a Psychiatric Consultant;
• care coordination and management;
• regular/proactive monitoring and treatment using validated clinical rating scales;
• and systematic psychiatric caseload reviews and consultation for patients who do not show clinical improvement.
What Resources are Needed for the Collaborative Care Model?
Below is a list of staff and resources needed to implement CoCM; please note this is not a complete list.
• A Behavioral Health Care Manager (BHCM) who is full-time or shared, employed or contracted, onsite or virtual;
• A contracted or employed Psychiatric Consultant (2-4 hours/week), onsite or virtual with protected time for the Primary Care Provider (PCP) and BHCM to review the caseload;
• Protected time for PCPs to periodically communicate and participate in the care coordination;
• A shared data registry that tracks depression scores, anxiety scores and progress in treatment for enrolled patients;
• Systematic screening protocols.
What is NC AHEC’s Role with Collaborative Care Model (CoCM)?
The North Carolina Department of Health and Human Services, Division of Health Benefits (DHB) has partnered with NC AHEC to provide educational and practice-based support to primary care practices interested in implementing the Collaborative Care Model. This includes coaching on workflows and billing/coding, registry implementation, and continuing education programs.
NC AHEC will offer CoCM virtual learning opportunities, including:
(1) Education Modules, designed for providers interested in learning about the CoCM. Modules currently available on demand include (listed in order of release date):
Module 17: Challenging Clinical Situations
Module 16: Tools for Financial Sustainability Using CoCM
Module 15: Improving CoCM Quality Using Technology
Module 14: Collaborative Care in Perinatal Populations
Module 13: Diversity, Equity, and Inclusion in Collaborative Care: A Review of the Evidence in Minority Populations and Next Steps
Module 12: Collaborative Care Model in Substance Use Disorders
Module 11: Primary Care Provider Engagement
Module 10: Best Practices in Pediatric Collaborative Care
Module 9: Behavioral Health Care Manager (BHCM) Best Practices
Module 8: Best Practices for Collaborative Care Management Behavioral Health Care Manager
Module 7: Brief Therapeutic Interventions
Module 6: Billing the Codes and the General Business Model for Collaborative Care
Module 5: The Role of the Psychiatric Consultant in the Collaborative Care Model
Module 4: Collaborative Care Management for Primary Care Providers
Module 3: Putting Collaborative Care Principles into Practice: Planning for Clinical Practice Change
Module 2: Laying the Foundation for Collaborative Care Through Practice Transformation
Module 1: Collaborative Care Model (CoCM) Rationale and Evidence
To register for and access the modules listed above, click the blue button below.
(2) Learning Collaboratives, designed for providers actively engaged with NC AHEC coaches to implement the CoCM within their practices.
Inaugural Collaborative Care Model (CoCM) Behavioral Health Care Manager (BHCM) Summit
May 16, 2024 | 9 am to 3:15 pm
McKimmon Center | Raleigh
1101 Gorman St, Raleigh, NC 27606
We are excited to announce the inaugural Collaborative Care Model (CoCM) Behavioral Health Care Manager (BHCM) Summit, presented jointly by NC AHEC and Southern Regional AHEC. Mark your calendars for Thursday, May 16 at the McKimmon Center in Raleigh, NC. Explore the pivotal role of BHCMs in CoCM and their significant impact.
This summit will feature esteemed national and state CoCM experts, including representatives from the AIMS Center at the University of Washington, as well as state government representatives. Attendees will benefit from insightful presentations by experienced CoCM BHCMs, integrated behavioral health Subject Matter Experts, university graduate education, and patient perspectives. Additionally, gain valuable insights from a primary care practice team that has successfully implemented CoCM in their clinic.
Don’t miss out on this invaluable training opportunity – register now! View the event flyer here.
What Other Groups Support CoCM?
Other agencies and associations that support this endeavor include:
• The NC Academy of Family Physicians, NC Pediatric Society, and NC Medical Society support this endeavor.
• Community Care of North Carolina (CCNC) provides access to an enhanced version of the AIMS Caseload Tracker registry for up to three years for qualifying practices starting in the fall of 2022.
• The NC Psychiatric Association and NC PAL are supplying adult and pediatric psychiatrists to partner with interested practices. NC PAL pediatric psychiatrists will be made available at no cost for up to ten practices.