The Preceptor Crisis: NC AHEC Addresses Increased Demand for Community Preceptors

As health care moves rapidly from hospitals to community settings, clinical education in community practices is increasingly important. However, over the last five years, new health science schools and increased enrollments have led to an approximate 40 percent increase in the demand for preceptors across the state, creating a statewide crisis in the availability of community preceptors—practicing clinicians in primary care and related disciplines who teach in community settings away from academic centers.
“All health science schools depend on community preceptors to help train their students, but they are increasingly becoming a scarce resource,”
noted Alan Brown, associate director of NC AHEC and a member of the Precepting Work Group. “Schools could not provide all the required clinical training experiences on-campus, and community preceptor settings offer a real-world perspective.”
The increase in demand for preceptors is exacerbated by significant changes in the time available for teaching, in compensation plans for clinicians, and challenges in preparing community clinicians for their faculty roles.
To address this statewide crisis in community precepting, the University of North Carolina Board of Governors convened a work group of educational leadership from a wide variety of institutions and professions to give recommendations for solutions. Facilitated by Warren Newton, MD MPH, director of the North Carolina Area Health Education Centers Program and vice dean of the UNC School of Medicine, with support from UNC General Administration, the Precepting Work Group submitted their recommendations to the UNC Board of Governors in early January 2018.
The work group’s plan considers priorities for public policy, recommending support for both public and private higher education institutions that produce clinicians who practice in the state and contribute to workforce diversity. In alignment with NC AHEC’s mission to improve the health and access to care of rural and underserved communities, the plan also emphasizes the importance of prioritizing practitioners who work in rural counties (as defined by the North Carolina Office of Rural Health) and those who work in community practices with substantial numbers of uninsured or Medicaid patients.
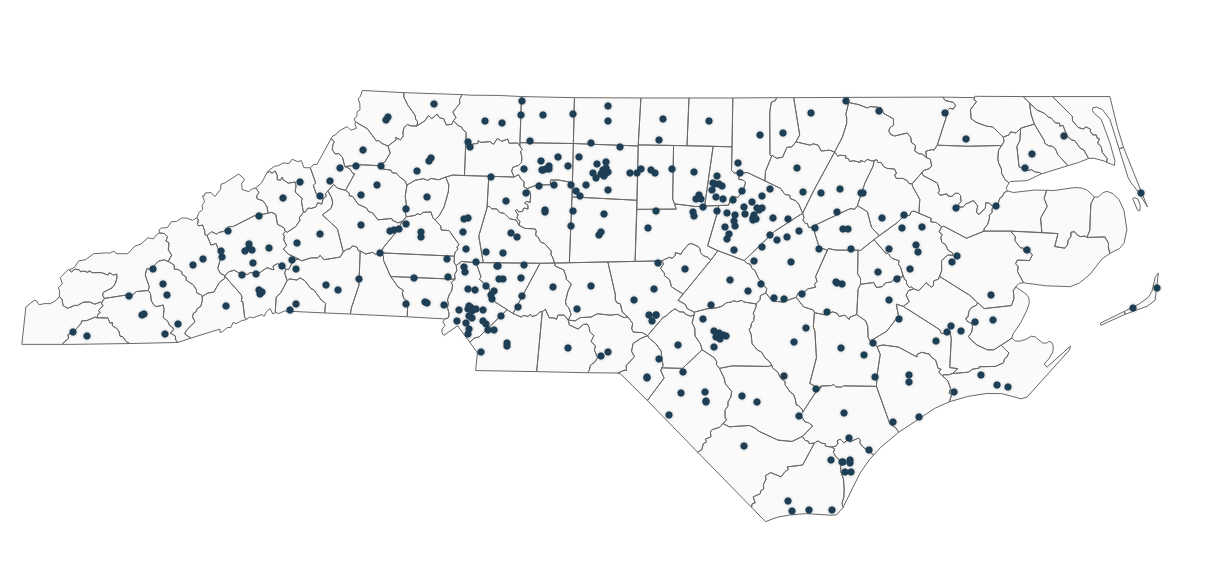
“NC AHEC works with all institutions and all health professions; our practice support team has worked with more than 1,200 primary practices, giving us a ringside seat to our state of health care,”
stressed Newton. “We have a convening role. It’s better that we all work together, better to hang together than hang separately. With the increasing rate of rural mortality, getting students into quality practices, doing work that matters, is key to North Carolina’s future.”
The plan recommends bold action to improve the quality of community-based health professions education, addressing both numbers and ongoing faculty development. The UNC Board of Governors approved the plan, which identified three courses of action related to community-based preceptors.
1) Pilot a tax credit for community-based health education preceptors.
The shortage in preceptors isn’t only a North Carolina problem, and offering a tax credit for preceptors isn’t a new concept. In 2014, led by their AHEC office, the state of Georgia was the first to pass legislation for a tax incentive program for preceptors. Maryland and Colorado quickly followed, and a number of states are actively pursuing similar efforts. Guided by the success of the tax incentive in other states, the work group recommends implementing a three-year pilot that would offer a tax credit to community-based clinicians who do not receive personal payments for precepting from any other source and who precept medical, nurse practitioner, nurse midwifery, and physician assistant students in primary care rotations from any North Carolina higher education institution. Each month, or 160 student-hours of precepting, would qualify for $1,000 tax credit, up to a maximum total of 10 student months annually.
“Currently, community-based education for health science students in North Carolina lacks statewide structure and coordination,” explained Brown. “Each school is challenged with securing an adequate number of community practitioners to precept students, resulting in growing competition that is often determined by which school can offer the highest financial incentive. While most preceptors teach out of a desire to give back to their professions, the financial implications are too strong to ignore.
“A statewide tax incentive would help reduce competition by standardizing the compensation rate.”
At a minimum, community preceptors would be encouraged to participate in annual faculty development, as provided or approved by their collaborating educational institutions. NC AHEC will work with preceptors and schools to provide verification of clinical teaching involvement and participation in faculty development. Leaders from the NC AHEC Program Office will devote 2018-19 to working with partner schools to operationalize the system, reporting to the UNC Board of Governors and the legislature on the progress and effectiveness of the tax credit program, including the long-term success in keeping students in North Carolina. After a formal review of the pilot program, the Precepting Work Group will consider extending the tax credit to community-based preceptors in pharmacy, nursing, allied health, and other health disciplines.
2) Develop a health education passport for all North Carolina health professional students.
Before starting each rotation, every student must meet the individual credentialing and orientation requirements of the host institution or community practice. Students are required to repeat these trainings and paperwork—criminal background checks and drug screenings, insurance and immunization forms, HIPAA and other medical record trainings—for each rotation, a time-consuming process for all involved. A common “passport” would streamline this process by facilitating discussion and agreement from all interested parties on standardizing these processes and forms.
This passport would allow student education at any community practice or hospital anywhere in the state, making it easier for students to complete the required onboarding process.
Building on the regional success of the Wake AHEC Consortium for Clinical Education and Practice (CCEP), which has already implemented this model for nursing and allied health students at many health care and academic institutions across the state, NC AHEC will work with all North Carolina health professional programs, health systems, and hospitals to develop uniform requirements. Student records and trainings would be available online and available anywhere in the state prior to clinical rotation. Individual institutions, practices, and professions may supplement this with specific information.
3) Support innovation in community health education through regional and statewide pilot projects.
NC AHEC will pilot several regional and statewide projects to support the first two parts of the Precepting Work Group’s plan, such as:
- establishing a statewide community preceptor faculty development program to offer joint online and in-person opportunities for preceptor development, shaped by the accreditation requirements of the different professions;
- launching a statewide academy of community educators working across schools and professions to provide support and educational development for community-based preceptors; and
- identifying and certifying exemplar teaching practices across the state that are committed to excellence in community-based health education and in measured quality of clinical care. In return for financial and other support, these practices will commit to teaching students most of the year, working with students from more than one profession, providing ongoing development of faculty and staff as teachers, and demonstrating excellent care as measured by access and chronic care metrics.
The plan’s approval by the UNC Board of Governors is an important first step in addressing the precepting crisis. Next steps will include disseminating the proposal among all community-based education partners and soliciting input from key stakeholders to develop a comprehensive proposal for the North Carolina legislature.
Follow NC AHEC (@ncahec) on Facebook and Twitter to keep abreast of the Precepting Work Group’s efforts to address the community precepting crisis in North Carolina.
About NC AHEC
The North Carolina Area Health Education Centers Program was established in 1972 to meet the state’s health and workforce needs. NC AHEC’s Program Office, nine regional centers, and the Duke AHEC Program provide educational programs and services that bridge academic institutions and communities to improve the health of the people of North Carolina with a focus on underserved populations. Visit ncahec.net to learn more about NC AHEC’s impact in your region.
